Scleral buckling is a time-tested yet underutilized technique for repairing retinal detachments. While many modern retina surgeons are moving away from it in favour of pars plana vitrectomy (PPV), scleral buckling remains an invaluable tool, especially for chronic and complex retinal detachment cases.
When performed by an experienced surgeon, scleral buckling offers:
- Fast recovery and minimal rehabilitation time
- A highly effective solution for chronic and complex retinal detachments
- A reduced need for additional surgeries, preserving long-term vision
At Prime Hospital, we believe in offering the least invasive yet most effective treatments for retinal detachments, ensuring the best outcomes for every patient.
A Brief History of Scleral Buckling
Scleral buckling has been a cornerstone of retinal detachment repair for over 70 years. It was first introduced in the 1950s by Dr. Charles L. Schepens, a pioneer in retinal surgery.
How It Revolutionized Retinal Detachment Treatment:
- Before scleral buckling, retinal detachment treatment was highly invasive and often unsuccessful.
- The introduction of scleral buckling provided a minimally invasive solution, dramatically improving success rates.
- Throughout the 1960s and 1970s, scleral buckling became the gold standard for treating retinal detachments.
Why Has It Declined?
With the rise of pars plana vitrectomy (PPV) in the 1980s and 1990s, many retina surgeons started shifting towards vitrectomy as their primary technique. However, despite this shift, scleral buckling remains a highly effective and relevant procedure, particularly for specific cases such as high myopia, chronic retinal detachments, and young patients.
Even today, in the right hands, scleral buckling delivers exceptional results, proving that some “old techniques” remain invaluable in modern ophthalmology.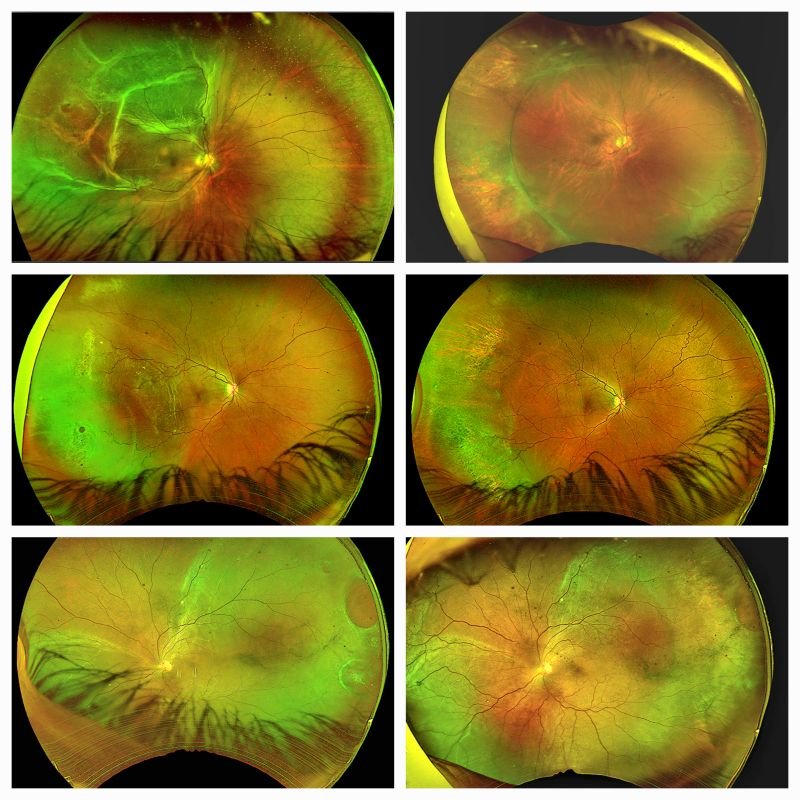
Understanding Scleral Buckling
What is Scleral Buckling?
Scleral buckling is a surgical procedure used to repair retinal detachments by placing a silicone band or sponge around the eye. This technique:
- Supports the detached retina externally by indenting the sclera.
- Reduces traction from the vitreous, helping the retina reattach naturally.
- Avoids the need for intraocular surgery, preserving the eye’s natural structure.
Why is Scleral Buckling Becoming Less Common?
Despite its effectiveness, scleral buckling is becoming less frequently performed due to:
- The rise of vitrectomy – Many retina surgeons now prefer PPV, as it is easier to learn.
- Longer learning curve – Scleral buckling requires specialized skills and precise preoperative planning.
- Limited training opportunities – Many new retina surgeons are not extensively trained in this technique.
However, for certain cases, scleral buckling remains the best approach—especially when performed by an experienced retina specialist.
The Advantages of Scleral Buckling
1. Ideal for Chronic and Complex Retinal Detachments
Scleral buckling is particularly effective for:
- Chronic detachments that have been present for an extended period.
- High myopia (severely nearsighted eyes), where the retina is thin and fragile.
- Proliferative Vitreoretinopathy (PVR) cases with large atrophic holes.
2. Faster Recovery & Minimal Rehabilitation
Compared to vitrectomy, scleral buckling:
- Preserves the vitreous, avoiding complications like cataract formation.
- Requires no strict post-operative head positioning like gas tamponade in vitrectomy.
- Allows faster return to normal activities with less post-op care needed.
3. Reduces the Need for Additional Surgeries
- Many vitrectomy cases require multiple interventions, while scleral buckling is often a one-time solution.
- It helps prevent recurrent detachment, making it a long-term success strategy.
Real-World Cases: How Scleral Buckling Saves Vision
Scleral buckling has proven its value in some of the most challenging retinal detachment cases. Below are three real-world examples where this time-tested technique provided life-changing outcomes for patients.
Case 1 – Chronic Retinal Detachment with Secondary Retinoschisis
Pre-Surgery:
A patient presented with a long-standing retinal detachment complicated by secondary retinoschisis (fluid-filled layers within the retina). No symptoms were present initially, leading to a delayed diagnosis and making the condition more complex to treat.
- The retina had been detached for months, increasing the risk of permanent vision loss.
- Secondary retinoschisis makes the retina thinner and more fragile, making vitrectomy less ideal.
- The patient had good visual potential, but without proper treatment, vision loss would have become permanent.
Surgical Approach:
- A scleral buckle was carefully placed, indenting the eye wall to close the retinal break and relieve traction.
- The retinal layers were allowed to settle naturally, avoiding aggressive intervention.
- The procedure was completed without removing the vitreous, preserving natural ocular integrity.
Outcome:
- The retina fully reattached within weeks, with stable vision post-surgery.
- The patient’s vision significantly improved, avoiding the need for further procedures.
- The secondary retinoschisis was resolved, confirming the effectiveness of an external approach without intraocular manipulation.
Lesson: For delicate, long-standing detachments with retinoschisis, scleral buckling offers a minimally invasive and highly effective solution.
Case 2 – Retinal Detachment in High Myopia
Pre-Surgery:
A patient with severe myopia presented with a progressive retinal detachment, detected early due to sudden-onset floaters and blurred vision.
- The retina was thin and stretched, making it prone to further damage.
- A vitrectomy could increase the risk of iatrogenic retinal tears or cataract formation.
- The patient was younger, making long-term preservation of the natural vitreous more desirable.
Surgical Approach:
- A custom-fitted scleral buckle was placed to relieve traction from the vitreous, allowing the retina to settle naturally.
- No intraocular intervention was needed, reducing risks associated with vitrectomy in high myopia.
Outcome:
- The retina was successfully reattached, preventing further progression.
- Preserved the natural vitreous, reducing future risks of complications like cataracts.
- Rapid recovery, with the patient returning to work within a week.
Lesson: Scleral buckling is an excellent first-line treatment for retinal detachments in high myopes, avoiding unnecessary vitrectomy-related complications.
Case 3 – 4-Year-Old Retinal Detachment with PVR
Pre-Surgery:
A patient presented with a 4-year-old chronic retinal detachment, which had already developed Proliferative Vitreoretinopathy (PVR)—a condition where scar tissue forms on the retina, making reattachment difficult.
- The detachment had caused severe visual impairment, with only light perception remaining.
- Large atrophic retinal holes had developed, complicating fluid drainage and retinal stability.
- PVR contracted the retina, making a vitrectomy alone unlikely to succeed.
Surgical Approach:
- A circumferential scleral buckle was placed, providing uniform support to the retina.
- Drainage of subretinal fluid was performed carefully to prevent further damage.
- Scar tissue was managed externally, reducing the risk of further contraction.
Outcome:
- Despite severe chronicity, the retina was successfully reattached.
- Some visual function was restored, significantly improving his quality of life.
- The eye remained stable post-surgery, preventing further deterioration.
Lesson: Even in long-standing cases with significant PVR, scleral buckling can provide a chance for retinal reattachment and vision preservation.
Why Choose Dr. Mandeep Lamba for Your Retinal Care?
Choosing the right specialist for retinal detachment surgery can mean the difference between saving and losing vision. Here’s why patients trust Dr. Mandeep Lamba:
- Retina Specialist with Extensive Experience – Expert in both scleral buckling and vitrectomy, ensuring the best approach for each case.
- Highly Skilled in Managing Complex Retinal Detachments – Special expertise in high myopia, PVR cases, and long-standing detachments.
- Patient-Centric Approach – Every case is individually assessed to choose the least invasive and most effective treatment.
- Access to Advanced Technology – Prime Hospital is fully equipped for advanced retinal imaging and surgical precision.
- Commitment to Vision Preservation – Prioritizing long-term vision stability with the right technique for each patient.
Conclusion: A Time-Tested Solution for Complex Retinal Detachments
Scleral buckling is not a dying art—it is a crucial tool in expert hands. While vitrectomy is the preferred method for many surgeons, scleral buckling remains the best choice for certain complex retinal detachment cases.
At Prime Hospital, we provide:
- Expert evaluation and treatment for all types of retinal detachments.
- A patient-first approach, using the least invasive yet most effective techniques.
- Specialized expertise in scleral buckling, ensuring superior outcomes.
If you or a loved one has been diagnosed with retinal detachment, don’t rush into an unnecessary vitrectomy. Consult Dr. Mandeep Lamba today and discover the best treatment plan for your eyes.
FAQs
Is scleral buckling still relevant in modern retinal surgery?
Yes! While vitrectomy is more commonly used today, scleral buckling remains the best choice for certain retinal detachment cases, especially in high myopes, young patients, and chronic detachments.
How long does recovery take after scleral buckling surgery?
Most patients recover within 1-2 weeks, with significantly less post-op rehabilitation than with vitrectomy.
Is scleral buckling better than vitrectomy?
There is no “one-size-fits-all” answer—scleral buckling is superior for some cases, while vitrectomy is better for others. A skilled retina specialist like Dr. Mandeep Lamba can determine the best option.
Can scleral buckling be combined with vitrectomy?
Yes, in some cases, a combined approach is used to maximize retinal stability and improve long-term results.
How do I know if scleral buckling is right for me?
A detailed retinal evaluation by Dr. Mandeep Lamba at Prime Hospital will determine the best treatment approach for your retinal detachment.



